Canadian chiropractors have positive attitudes toward evidence-based practice (EBP).[1]
What is evidence-based chiropractic care?
That said, if you ask Ontarians, including chiropractors and other health care professionals, how they define evidence-based chiropractic care, you’ll hear a range of answers.
This scenario is not new. Since the inception of the evidence-based medicine movement in the early 1990s, there’s been extensive debate within health care professions about ‘what’ evidence-based care should entail in practice.[2]
Mixed perceptions of evidence-based chiropractic care also raise questions, such as:
- What role do patient values and preferences play in the planning and delivery of evidence-based care?
- How do clinicians discover patients’ values and preferences and what happens when they conflict with best available research evidence?
- What are the barriers to successfully integrating research evidence into clinical practice and how can they be overcome?
These challenges underscore the imperative to support better patient care and advance the profession through a shared understanding or framework around what exactly ‘evidence-based practice (EBP)’ means for chiropractic care.
OCA Evidence-Based Framework Advisory Council (EBFAC)
As part of our association’s mission to advance the understanding and use of chiropractic care, we are leading this important work.
To draw on a wide range of experienced practitioners’ expertise, we created the OCA Evidence-Based Framework Advisory Council (EBFAC). Comprised of 13 members, it represents a diverse cross-section of chiropractors engaged in clinical practice, as well clinical and/or basic sciences research, and a patient.
What are the EBFAC’s Goals?
1– Develop a comprehensive and inclusive definition of chiropractic care
Our first goal is to explore the evidence-based framework to develop a comprehensive and inclusive definition of chiropractic care. Up until now, we’ve been significantly focused on high-quality research and guidelines to support low back pain as the key area that chiropractors treat, even though we know they contribute to much more.
Based on clinical expertise, scopes of practice and other evidence, we know chiropractors are also effectively treating other parts of the spine, joints and related nervous system, such as neck and shoulder pain, as well as chronic conditions like arthritis.
Part of this goal is also to increase stakeholders’ understanding of spinal manipulative therapy or adjustments, as well as other chiropractic treatments, and how they help relieve a person’s pain and improve their function.
2 – Identify and gain a clearer understanding of research priorities to fund
Our second goal is to leverage this work to help us identify and gain a clearer understanding of the research priorities our association should fund. As we move forward with our research agenda, this work will build on the important work of the Canadian Chiropractic Guideline Initiative (CCGI) and the Canadian Chiropractic Research Foundation (CCRF) to provide needed support in a timely manner.
3 – Strengthen OCA support for ‘knowledge translation’
Our final goal is to strengthen our support for ‘knowledge translation,’ which is the two-way process of integrating emerging research into clinical practice and using clinicians’ questions and challenges to help inform research. Strengthening knowledge translation across the chiropractic profession will help our members enhance patient care, while it continues to generate new evidence.
Together, we can expand research and amplify knowledge translation to set a new direction for the profession in terms of advocacy and the research agenda. Achieving these latter two goals should also help us and our chiropractic members understand how to better partner with key stakeholders in the chiropractic ecosystem.
Enhancing Interprofessional Collaboration and Outcomes
Having a comprehensive and inclusive definition for chiropractic care will give us a common language and tools that enable chiropractors to interact more with physicians, as well as nurse practitioners. This will help pave the way for chiropractors to share their evidence-based plans of care with these primary care providers.
Currently, patient referrals from physicians and nurse practitioners often go to health care professionals covered by Ontario’s publicly funded system. I think a shared understanding of evidence-based chiropractic care will also build confidence among those primary care professionals to refer patients to chiropractors and include them in their circle of care.
Appropriate inclusion of chiropractors in a patient’s circle of care enhances patient outcomes. In fact, in its ‘Prescription for Ontario,’ the Ontario Medical Association (OMA), stated that “Patients do better when they have a team of care providers, including not only family doctors and specialists.” Furthermore, this report suggests “Where these teams exist, patients have faster and easier access to specific care they need so are healthier, have fewer hospital admissions and are more satisfied. System costs are also reduced.”[3]
Understanding the science behind chiropractic care should also open opportunities for chiropractors to collaborate with other regulated health professionals and neuromusculoskeletal (nMSK) experts like rheumatologists and physiatrists to further enhance patient outcomes.
Beyond health care professionals, a shared definition of evidence-based chiropractic care will also help us effectively communicate with payers, like extended health care (EHC) benefits insurers, about how chiropractors deliver care and its benefits to patients. And an enhanced understanding of chiropractic care may also help these insurers better understand the value of aligning EHC plans with nMSK guidelines, as explained in my last post on helping Ontarians access the care they need.
Raising Patients’ Understanding
Beyond helping more patients access needed care, enhancing it and improving their outcomes, this work will also give us new evidence-based tools to better educate patients on their options.
With a comprehensive definition, chiropractors can explain the breadth of care that chiropractic care delivers, from assessment and diagnosis to prescribing exercises and other therapies and why care is delivered the way it is.
And it will help patients better understand that chiropractic care involves more than spinal manipulative therapy or the spinal adjustment. That said, this framework can be used to provide the evidence that adjustments are a safe and effective intervention, while dispelling misconceptions.
For patients, it’s also important that others in their circle of care like their family doctor or rheumatologist, understand how chiropractors can support their condition.
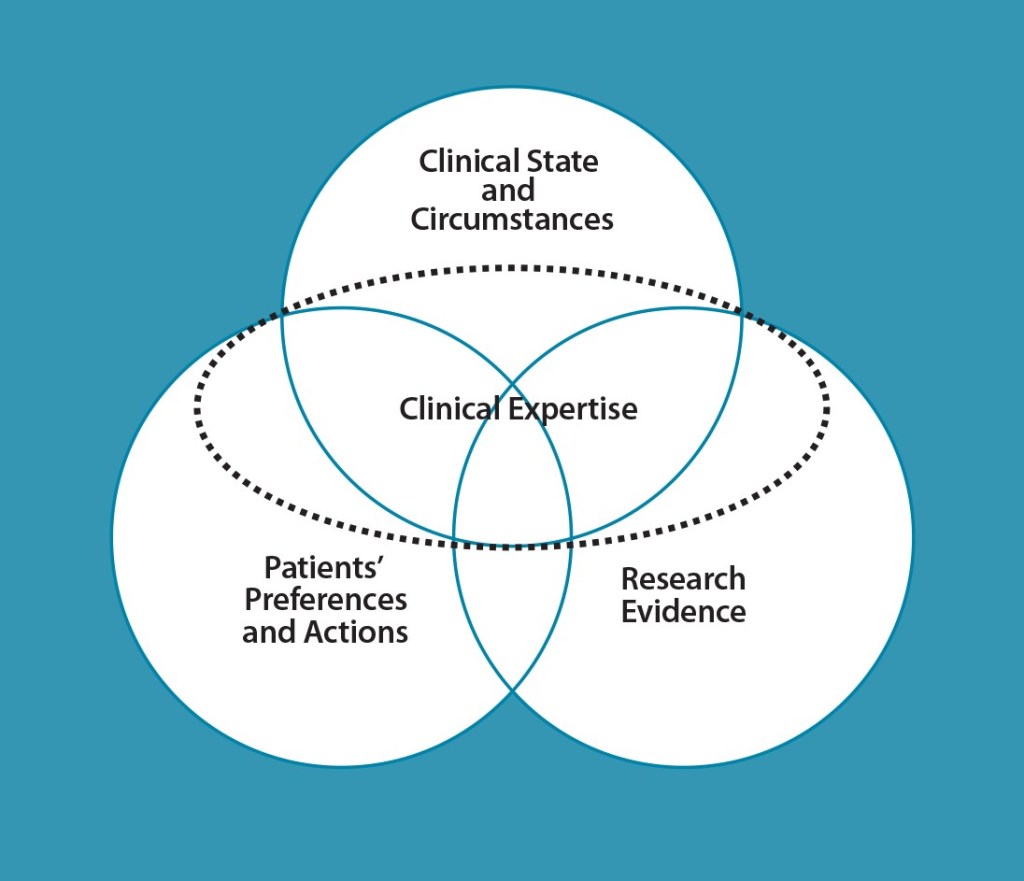
Haynes Model for Evidence-Based Practice
One of the EBFAC’s first priorities was to identify the most effective model of evidence-based practice to underpin its work. Following a thorough review of several options, it adopted the Haynes four-part model, which views clinical expertise as the lens to integrate the three components of:
- Patients’ preferences and actions
- Clinical state and circumstances
- Research evidence [4]
This model describes what evidence-based practice ought to look like but not necessarily its actual state.
Based on the Haynes model and its elements, the EBFAC will develop a series of research papers on evidence-based chiropractic practice and a decision aid to help guide clinical chiropractic judgment in instances where little or no high-quality research evidence exists.
In developing these papers, the EBFAC is integrating leading Canadian and international researchers’ expertise, as well as exploring leading practices from other professions globally. Its work also aligns with the work of the World Federation of Chiropractic’s EPIC model of care – bringing our profession in line with global health care best practices.[5]
Starting with Patient Preference
When the EBFAC first met in early 2020, there was an almost immediate consensus that this work must benefit patients.
And we know the voice of patients in Ontario is very powerful in effecting change, as we’ve seen over and over again. That’s likely why key organizations that drive quality in health care, such as Health Quality Ontario, have started to prioritize the voice of patients. For example, they’ve integrated patient preferences in their work, such as developing practice guidelines or advice for clinicians.
Yet patient preference is one of the least explored and least understood elements in the evidence-based framework model.
In fact, up until recently, it was felt that only focusing on the best available evidence was what mattered. With their preference given a low priority, many patients weren’t complying with care plans and subsequently, they weren’t getting the outcomes they were looking for. So, in Ontario, there’s now a growing recognition of the voice of patients in influencing care, advocacy and policy.
As enhancing the patient experience including outcomes is our priority, patient preference was an important place for us to begin our investigation of the Haynes model components in an in-depth manner.
The EBFAC is currently focused on developing research papers that explore patient preference and other evidence-based practice components, along with pertinent scenarios. Our intention is to release these papers and the decision aid concurrently, so they serve as robust, integrated resources to support all chiropractors in the science and art of practice.
But these resources are just the beginning. We will build on them to develop programming and partnerships to evolve the chiropractic profession, provide supports to our members and ultimately enhance patient-centred care.
While this work will benefit various stakeholders, I think it will provide the most value to patients with spine, muscle, joint or related nervous system conditions.
I look forward to sharing the EBFAC’s work, as it evolves, and my perspectives with you. And as always, I welcome your feedback.
[1] Bussières A.E., Terhorst L., Leach M., Stuber K., Evans R. & Schneider M.J. (2015). Self-reported attitudes, skills and use of evidence-based practice among Canadian Doctors of Chiropractic: a national survey. The Journal of the Canadian Chiropractic Assoc. 59(4). 332-348.
[2] Guyatt, G., Cairns, J., Churchill, D., et al. (1992). Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 268(17). 2420-2425.
[3] Ontario Medical Association (OMA). (2021). Prescription for Ontario: Doctors’ 5-Point Plan for Better Health Care. 45.
[4] Haynes, R.B., Deveraux, P.J. & Guyatt, G.H. (2002). Clinical expertise in the era of evidence-based medicine and patient choice. BMJ Evidence-Based Medicine. 7. 36-38.
[5] World Federation of Chiropractic. (2019). Quarterly World Report.




 Boards and CEOs bear enormous responsibility for the well-being of their organization’s people. In turn, organizations rely on fully engaged and motivated employees to deliver on their mission. Much is written about how ‘trust’ affects each employee’s engagement. Employees should be able to trust their organization to provide a safe environment that evokes pride and provides ample support for them to thrive in delivering quality work to the communities they serve. Employees are also expected to share values aligned with their organization and to come to work each day prepared to do the best they can. Informed leaders know that most employees share this goal. So when employee performance goes amiss, it’s frequently because the culture, including the systems, processes and tools, impedes their success.
Boards and CEOs bear enormous responsibility for the well-being of their organization’s people. In turn, organizations rely on fully engaged and motivated employees to deliver on their mission. Much is written about how ‘trust’ affects each employee’s engagement. Employees should be able to trust their organization to provide a safe environment that evokes pride and provides ample support for them to thrive in delivering quality work to the communities they serve. Employees are also expected to share values aligned with their organization and to come to work each day prepared to do the best they can. Informed leaders know that most employees share this goal. So when employee performance goes amiss, it’s frequently because the culture, including the systems, processes and tools, impedes their success.

 Leadership has been fundamental to our accomplishments for as long as we have shared stories of our successes and failures. Coordinating work or rather making the best use of an organization’s assets and the skills of its people, along with engaging everyone to advance a better future, drives us as human beings.
Leadership has been fundamental to our accomplishments for as long as we have shared stories of our successes and failures. Coordinating work or rather making the best use of an organization’s assets and the skills of its people, along with engaging everyone to advance a better future, drives us as human beings. In my first
In my first  In just over a decade, Ontario is expected to see its number of seniors, 85 years and older, quadruple. As Ontarians age, they also develop more comorbidities, with 70 per cent of seniors expected to live with two or more chronic conditions by 2030. For these frail patients requiring services from multiple providers, accessing the right level of care at the right time is bound to be tricky.
In just over a decade, Ontario is expected to see its number of seniors, 85 years and older, quadruple. As Ontarians age, they also develop more comorbidities, with 70 per cent of seniors expected to live with two or more chronic conditions by 2030. For these frail patients requiring services from multiple providers, accessing the right level of care at the right time is bound to be tricky. ow that to help our patients achieve what’s most important to their wellbeing, we need to bring clinical care and
ow that to help our patients achieve what’s most important to their wellbeing, we need to bring clinical care and